Multi-Agency Protocol for the Management of Unexpected Childhood Deaths
Table of Contents
1. General
1.1 Introduction – The Joint Agency Response [1]
The Cambridgeshire and Peterborough Safeguarding Partnership have adopted this protocol. Its purpose is to support professionals and organisations to work together in a coordinated way when a child has died unexpectedly. The document ‘Protocol and Terms of Reference for the Child Death Overview Panel for Cambridgeshire and Peterborough Safeguarding Children Board details how information about all child deaths in Cambridgeshire and Peterborough are collated and analysed by the Child Death Overview Panel. All professionals should follow the protocol in collaboration with relevant agency specific policies, procedures, and protocols.
This protocol details the operational ‘Rapid Response Process’ ‘which should be initiated when a child dies unexpectedly’. The unexpected death of a child is traumatic for everyone involved. The family will experience extreme grief and shock and professionals will need to support them sensitively. Unexpected deaths must be fully investigated to identify contributory factors and prevent future deaths. The investigation needs to balance medical management with care and support of the family, potential safeguarding concerns and an understanding of the cause of death.
1.2 Aims
Professionals need to work together in a coordinated way to:
- Establish the cause of death including whether a crime has occurred
- Support the family
- Identify contributory factors which might prevent future deaths
- Gather information to contribute to the Child Death Overview Panel arrangements
- Identify potential safeguarding concerns
Knowing how and why a child died may offer comfort to parents and families and lessen a natural tendency to blame themselves. Professionals who understand about contributory factors may be able to use this information to prevent future deaths.
Over 5000[2] children die in the UK each year, a very small number of these will have a malicious or non-accidental cause. Examining all childhood deaths will help to highlight these cases and help inform the Department of Health about the risk factors.
The Safeguarding Childrens Partnerships have a responsibility to ensure a coordinated response by partner agencies to the unexpected death of a child. Together with reviewing all child deaths, this information can advise local strategic planning about the modifiable factors, which may prevent future deaths.
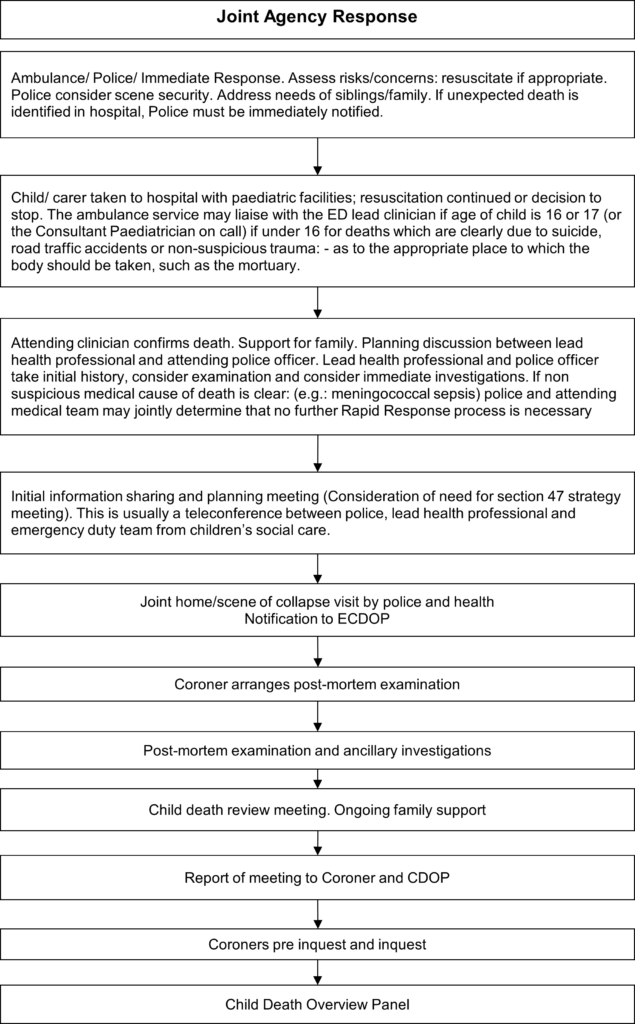
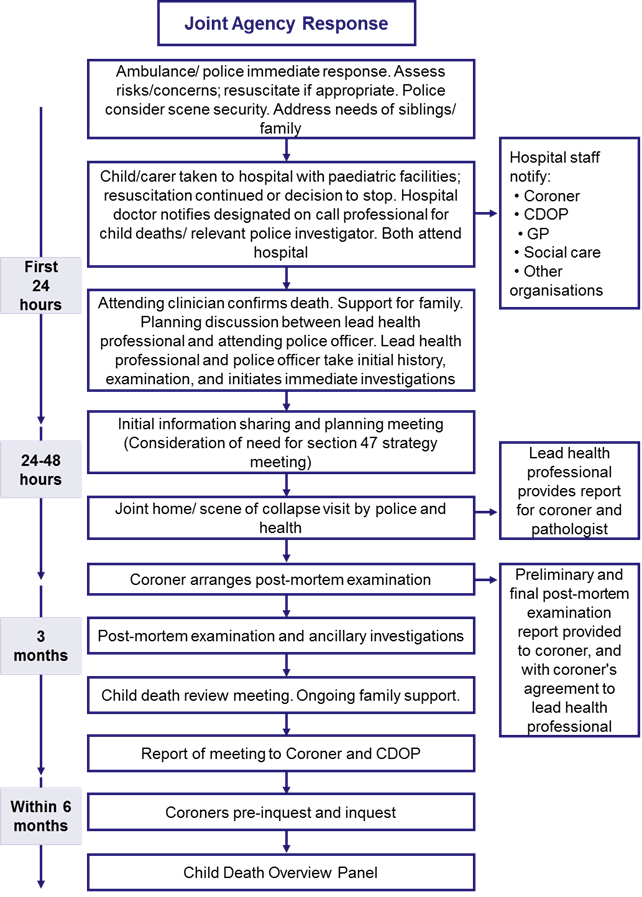
1.3 Processes
1.4 Statutory Implications
The protocol is based on the guidance in Chapter 5 of Working Together to Safeguard Children: July 2018; and following the principles of Sudden and Unexpected Death in Infancy and Childhood, multi-agency guidelines for care and investigation 2016
1.5 Definitions
Child.
All young people who have not yet reached their 18th birthday, including those living independently, in further education, employment, a member of the armed services, in hospital, in prison or a Young Offenders Institute. It includes the death of all children where a birth certificate has been issued but excludes all planned terminations. It includes the case of stillbirth where no healthcare professional was in attendance.
Parent.
The adult or adults with legal “care and control” of the child at the time of death with ‘parental responsibility’ (PR) for the child. PR may be shared with the Local Authority through a care order or given to an adult through legal process such as adoption. Any person with PR whether caring for the child or not at the time of death will be deemed to be a ‘parent’.
Sudden Infant Death Syndrome (SIDS).
The sudden death of an infant less than one year of age, which remains unexplained following thorough case investigation, including complete autopsy, examination of the death scene and a review of the clinical history.
Sudden Unexpected Death in Childhood (SUDC).
The sudden death of a child over 1 year, up to 18 years, which was not anticipated as a significant possibility 24 hours before death. Alternatively, where there was an unexpected collapse leading to, or precipitating, the events that led to the death.[3]
Sudden Unexpected Death in Infancy (SUDI).
The sudden unexpected death of a child under the age of 12 months.
2. Responsibilities
2.1 Joint responsibilities
Agencies are required to identify staff to undertake their normal tasks as well as working together as a multiagency team following the death of a child. This team will be coordinated by either a police officer or health professional:
- Ensuring that bereaved families are treated with sensitivity and respect, offered appropriate support and kept fully informed
- Adopting an open minded and proportionate and professional approach to circumstances
- Ensuring that evidence is preserved (such as the last nappy) and that the death is thoroughly investigated
- Providing a prompt response and ensuring that the investigation is completed expeditiously
- Respond quickly to the unexpected death of a child.
- Undertake immediate enquiries into the death and evaluate and interpret the available information.
- Make enquiries or investigations, which relate to the responsibilities of their organisations when a child dies unexpectedly including liaising with those who have ongoing responsibilities for surviving family members, (particularly siblings)
- Collect information to inform the Coronial process.
- Collect information for the Child Death Review process
- Maintain close liaison with family members and other professionals working with surviving family; ensure they are apprised of results of enquiries. This should be done by a named keyworker.
- On occasion, it might be appropriate to seek consent to examine family members’ medical notes.
- Cooperate with an investigation by the Prisons and Probation Ombudsman if the child died in custody (or by the Independent Police Complaints Commission in the case of police custody)
2.2 Evidence of Criminality
In most situations’ professionals will have no reason to suspect a death involves a criminal act. However, should there be any suspicion a child has died from an unlawful act, then the presumption shall be that the child’s body and the place of death are both crime scenes. These will need to be secured pending the arrival of a Police Senior Investigating Officer. Whilst every effort will always be made to resuscitate a child, if it is clear no medical intervention can help, the crime scenes must be secured as soon as possible.
If a criminal act is suspected, immediate consideration must be given to whether or not there are other children e.g. siblings who may require safeguarding and a referral made to children’s social care.
2.3 Notifications to Coroners
The Coroner must be notified of a body lying within his jurisdiction when:[4]
- The child died a violent or unnatural death.
- The death was sudden death or of unknown cause.
- The child died in prison.
A body cannot be moved across jurisdiction boundaries without the coroner’s permission. However, with prior permission Coroners will accept the removal of a body to an Emergency Department in accordance with this protocol.
The Coroner must be notified by the Police or attending clinician depending on circumstances of death. Both must assure themselves that the notification has been made or undertake the notification themselves.
All information about the circumstances of the death, including a review of all medical, social and education records, must be included in the report for the Coroner.
2.4 Record Keeping
Records are essential to the learning process, underpinning decision making and potentially for court proceedings; therefore, accurate records must be kept of all tasks undertaken as directed by this protocol.
- Decisions must be recorded, together with reasons.
- All records must be legible, timed, dated and signed by the author.
- A record of what was said by parents and carers will need to be made and remarks attributed to a named person.
- Opinion needs to be distinguished from fact.
2.5 Coordination of Rapid Response
- The Child Death Review (see 1) notes the ‘Designated Paediatrician with responsibility for unexpected deaths in childhood’ has lead responsibility for most of the processes detailed in the guidance. This is set out in 3.7
- The CDOP Manager will support the Designated Paediatrician in ensuring that the child death review arrangements are followed.
- All agencies that have been involved with the child (before and after death) are expected to cooperate fully with the coordinator and the lead professional for the Joint Agency Response process.
2.6 Individual Agency Responsibility
Individual agencies are encouraged to develop compatible guidance for their staff. This should be ratified by the Child Death Overview Panel to ensure that it is compatible and consistent with this protocol.
2.7 Adjoining Counties
Occasionally children from Cambridgeshire or Peterborough are cared for, or hospitalised “out of County”, alternatively a child “out of County” is transferred to a Cambridgeshire or Peterborough hospital or carers. The principle to be followed is, whilst for the Coroner the place of death determines responsibility, it is the child’s usual home address which determines the responsible authority for the Child Death Review Process. When an unexpected child death occurs within the Cambridgeshire and Peterborough area, the police will be responsible for the initial notification of the death to the home area. Subsequently the CDOP Manager will liaise as appropriate.
In order to avoid omission notification to home CDOP. Agencies should err towards duplication of notification: to both Home CDOP and CDOP local to the place of death.
3. Responding to the unexpected death of a child
3.1 General Principles
This protocol cannot predict all circumstances relevant to an individual death; rather it sets out guidelines and principles to follow as circumstances dictate. However, staff must be mindful that most of this guidance is statutory, therefore departures from it will need to be documented with a rationale.
The principles applied are.
- This protocol is applicable to unexpected deaths in children, of any natural, unnatural or unknown cause, at home, in hospital or in the community.
- It excludes those babies who are stillborn (where a medical professional was present) confirmed and planned terminations of pregnancy carried out within the law.
- Where the cause of death is obvious, e.g. a road traffic collision, some consideration should be given to the events leading up to the death; for example, a young unsupervised child who is killed may need further investigation.
- Children with Life Limiting or Life Threatening (LL/LT) conditions are as valued and important as any other child. The application of this protocol should be considered, and the response should be appropriate and supportive.
The protocol is applicable for deaths of children across the Cambridgeshire and Peterborough area, irrespective of their home address. The Children and Social Work Act 2017 Legislation allows for Child Death Review (CDR) partners to make arrangements for the review of a death in their area of a child not normally resident there. A pragmatic approach should be taken to such deaths, entailing discussion between the CDR partners in the area where the child is normally resident and those in the area where the child died. In all cases, the CDR partners in the area where the child is normally resident is responsible for ensuring that a review takes place at CDOP level. Consideration should also be given to where the most learning can take place, and this may sometimes dictate that a different CDOP to the area where the child is normally resident leads the discussion.
- To achieve a balance between forensic and medical requirements with the family’s need for support.
- Children with an existing disability or medical condition where the death is not anticipated, have the same level of review as any other child.
- If a death is anticipated due to a known illness, it should only be subject to this protocol if there are reasons to be concerned about the circumstances of their death.
- If abuse or neglect is suspected as a cause of death or as a contributory factor, immediate consideration must be given to the safety of siblings.
3.2 First Response, Ambulance staff, GP, Fire & rescue
At the scene of an unexpected death, the first responsibility is the preservation of life; the second is a duty to safeguard other children. Resuscitation should always be initiated unless it is inappropriate to do so because resuscitation is clearly futile. Ambulance staff should:
- Attempt resuscitation in all cases unless there is a condition unequivocally associated with death or a valid advance directive. That is, do not automatically assume death has occurred.
- Clear the airway and, if in any doubt about death, apply full Cardiopulmonary Resuscitation.
- Inform Emergency Department of estimated time of arrival and patient condition.
- Take notes about how body was found, including anomalies/inconsistencies of accounts and marks/injuries and discuss these with the police.
- Deaths which are clearly due to suicide, road traffic accidents or non-suspicious trauma: – bodies should be taken to the appropriate place, such as the mortuary.
Where resuscitation is clearly inappropriate it is usually still desirable to take the child to hospital. The only exception to this may be the designation by the police of a crime scene.
Most other actions from this protocol follow the child’s removal to an emergency department in the hospital.
3.3 Hospital Staff in Emergency Department
Most children will be taken to the nearest emergency department. The Emergency department staff will be responsible for assembling a resuscitation team, including on call paediatric staff for children under the age of 16 and to promote ongoing care and family support. On arrival at ED.
- All information gathered by the Ambulance crew or GP should be shared with the medical staff taking over responsibility for the child.
- On arrival the child should be taken to an appropriate room for the continuation of resuscitation if appropriate. However, if the Child is dead then this is declared.
- Parents should be given the choice of remaining with their child whilst resuscitation is attempted or be allowed to go to a private room and be kept fully informed as to what is taking place.
- Staff should be sensitive to the needs of the parents and ensure they refer to the child by name and in the present tense.
- If possible, a nurse is appointed to act as an interface between the family and the medical team attending to the child and to support them through the process at the hospital when the child dies.
- If possible, the Doctor in charge will consult with parents about deciding how long resuscitation should continue.
- If there are suspicions that the child died from an unlawful act, immediate consideration should be given to the need to safeguard any remaining siblings and Social Care must be contacted immediately.
3.4 Assessment and Investigation following admission to the Emergency Department
In all cases:
- A senior doctor should take a detailed and careful history of events leading up to and immediately prior to death. See practice note in Appendix B for details. If the Senior Investigative Officer (SIO) is at the hospital, consideration should be given to a joint interview where appropriate. This should not delay the taking of a history from parents / carers.
- Medical notes should record conversations with parents with particular attention paid to ensuring which comments are attributable to which parent. Ideally contemporaneous notes with a verbatim account should be documented.
- A thorough examination of the body by a senior doctor should take place with the examination findings recorded on a body chart (including any post mortem changes), unless agreed between lead health professional and lead investigating police officer, for example if it is a death which is clearly suicide, road traffic accident or non-suspicious massive trauma. If the SIO is at the hospital, consideration should be given for this to take place with the SIO present. This should not delay examination of the body. A clear example of where this should happen would be SUDI.
- Responsibility for notifying the Coroner will fall to the doctor confirming death or the Police (SIO).
In a SUDI case the following specimens must be taken.
- Nasopharyngeal Aspirate – Virology to be taken in ED
- Pharyngeal swab – Microbiology to be taken in ED
Plus, the following sample may be taken.
- Additional samples as approved by the Coroner according to local protocols – See appendix A and B. Essentially this would constitute one attempt at a lumbar puncture and a cardiac stab for blood cultures, with an expectation that the pathologist would undertake any other necessary investigations at post-mortem.
- As with all clinical scenarios – it is the role of the doctor to try to make a diagnosis. If specific tests are suggested by the history and/or examination (which are not otherwise covered above), then these may be undertaken, particularly if it is thought that deferring the tests to post-mortem might be clinically unhelpful. An example of this might be a high suspicion of an inherited metabolic disorder.
Any further investigations should only be commissioned following the initial case management discussion to meet an identified investigative or clinical need.
3.5 Family Support
When the child has been pronounced dead and resuscitation has discontinued.
- The most appropriate senior clinician should firstly review all available information, and then break the news to the family. The news should be delivered in a private room with the allocated nurse present.
- Intravenous cannula, endotracheal tubes and other equipment may be removed from the child, but this should be documented clearly in the notes and countersigned by staff member to confirm that the items were removed as documented in the notes. The counter signatory should be a fellow professional not involved in the immediate care of the child.
- Any nappies or clothing should be removed and sealed in a plastic bag and should accompany the body to the mortuary.
- The child’s face should be cleaned, and the child dressed in a clean nappy and wrapped in a shawl or blanket.
- The parents should be allowed to hold their child, unless the Police object to the proposal.
- Ask parents if they wish to have a footprint/handprint or a lock of hair by way of a keepsake. This should be offered early but made clear to parents that they may not be able to receive this straight away. Whilst such a hair sample would technically be a sample under the Human Tissue Act (2004), common sense should prevail, but in all cases it will be necessary to discuss with the Police and Coroner who will endeavour to meet reasonable requests wherever practicable. Care needs to be taken to handle the child gently.
- In rare cases when deliberate harm is suspected DO NOT take hand or footprints, the pathologist will do this later on request.
- If the family request that the baby be bathed for cultural reasons, permission should be gained from the SIO and Coroner before agreement.
- The family should be advised the death will be reported to the Coroner and that for all unexpected deaths a post-mortem examination may be carried out. The family should be informed that the cause of death will not be known until after the results of the post-mortem are analysed.
- At this point the family should be given relevant information depending on the age of the child including
- for infants – Lullaby Trust leaflet
- for all children the CDOP leaflet “the child death review”
See Appendix C for contact details for bereavement organisations. Each hospital has its own bereavement department.
3.6 Role of Health professionals
3.6.1 On call Health Professional
If a child dies unexpectedly at home or non-hospital setting, the professional confirming death should contact the Police at the earliest opportunity through calling the police control room on 101. If there are concerns that the death may be suspicious 999 should be called. As soon as possible, the police should follow the protocol above and make telephone contact with the health professional named on the on-call rota. Between the police and the health professional they will identify the person to instigate the information sharing meeting, home visit and information collection and provide support to family. If it is decided a home visit will not take place, then the reason for this is taken at the information sharing meeting and recorded.
If there are suspicions the child had died from an unlawful act, the scene must be secured at the earliest opportunity, and ‘handed over’ to the first Police officer to attend. Any suspicions must be reported to the Police and the receiving Doctor in the ED at the earliest opportunity.
The health professional on the on-call rota for unexpected death in childhood will be a senior health professional with appropriate knowledge and training.
The on-call period for phone cover is between 8am and 8pm each day including weekends and bank holidays with home visits carried out between 9am and 5pm. The frequency of being on-call is determined by the number of health professionals engaged in this process.
The on-call health professional is to liaise with the police SIO as soon as possible once they become aware of an unexpected death of a child, irrespective of where the information came from. The purpose of this discussion is to share information regarding the death and identity of the child, to discuss the planning of a joint scene of death visit with the police and discussion with the parents. The health professional also needs to inform the CDOP Manager via the eCDOP public site: https://www.ecdop.co.uk/CambridgeshirePeterborough/Live/Public as soon as possible to enable further gathering of information and continuity of the process. The eCDOP system uses the statutory forms and process from the Working Together 2018 guidance and assists safeguarding teams to ensure compliance. The eCDOP system automatically transfers data at each relevant stage of the process into the National Child Mortality Database (NCMD). This information is then used to analyse data nationally in order to improve learning and implement strategic improvements in health care for children in England, with the overall goal to reduce child mortality. There may be a need to attend a child protection strategy meeting if required. See section 4.0 for further details on scene of death visit.
Record management must be factual, completed contemporaneously, signed and dated. Documentation completed following a scene of death visit and discussion with the parents must be shared with the pathologist within 24 hours of the visit if during the working week. Form B should also be completed and sent to the CDOP Manager. This will be requested by them via eCDOP.
3.6.2 Designated Doctor for Child Death
The Designated Doctor for Child Death is at the heart of this process. In Cambridgeshire and Peterborough parts of this role may be delegated to the health professionals on the rapid response on call rota. The responsibilities include ensuring systems are in place to:
- Advise the CCG on commissioning clinicians with expertise in undertaking enquiries into unexplained deaths plus availability of relevant investigative services of radiology, laboratory and histopathology services.
- Coordinate the team to respond to each unexpected child death in accordance with this protocol.
- Liaise with the consultant clinician dealing with the death.
- Ensure relevant professionals are informed of the death and begin to gather information (e.g.: police, social care, GP, health visitor or school nurse).
- Convene multi-agency case discussions potentially by phone when initial post-mortem results are available.
- Ensure appropriate attendance at the multi-agency case discussions when the final post-mortem results are known and ensure that the collection of information is completed for the data set form C.
- Support the CDOP chair and the panel to deliver the rapid response protocols; identify training and communication needs across Cambridgeshire and Peterborough for professional staff.
3.6.2 Senior clinician dealing with the death
The Senior clinician dealing with the death (Consultant Paediatrician or ED Consultant, usually the former for children under 16 years old) has responsibility to:
- Provide clinical care.
- Examine the child’s body (see appendix A and B)
- Take a detailed history of events leading up to and following the child’s death from the parents. Review all available information. Fully record all information.
- Inform the parents about the death.
- If appropriate, inform parents a post-mortem will be carried out and that a Coroner’s officer will be contacting them with more information.
- Liaise with the Police about the death.
- Initial information sharing with relevant agencies as soon as possible:
- other health professionals e.g. GP, professional certifying death
- local authority children’s services (social care)
- Child health records
- Consider a referral to Children’s Social Care if there are child protection concerns
3.7 Role of Police
National Guidance [a] requires an Officer of at least the rank of Detective Inspector to attend all reported cases of sudden and unexpected deaths of infants. Within Cambridgeshire Constabulary this falls to a Detective Inspector or above, who has undergone specific training to ensure they are equipped with the appropriate skills and knowledge to lead, manage and guide the Police response and investigation into the sudden unexpected death of a child. Every report of the unexpected child death received by Police will immediately be allocated to one of the specialists ‘on call’ Senior Investigative Officers (SIO) who has responsibility to respond to such incidents.
The specialist ‘on call’ SIO will be advised by the Force Control Room whenever they receive a report of a sudden unexpected child death. The SIO will attend the scene and/or the Accident and Emergency Department as circumstances require – but they will always be contactable via the Force Control Room (01480 426001 Duty Control Room Inspector – restricted number) in any circumstance where this protocol applies.
The SIO has responsibility for conducting a large number of ‘fast track actions’ in order to manage the initial stages of the investigation into understanding why the child died. It is important that other partners are aware of these actions since they may be asked to assist in the discharge of these actions or, alternatively, they may benefit from knowing the nature of the information the Police will be collecting.
The SIO will contact the health professional on the Rapid Response on-call rota as soon as is practicable. The purpose is to instigate the Rapid Response procedure, informing Health of the child’s death and to coordinate where applicable a visit jointly performed by health and police professionals to the scene of death. If this joint visit does not occur, the rationale for this decision will be documented and reported at the information sharing and management meeting. If further clarity is needed, the Designated Paediatrician with responsibility for the unexpected deaths in childhood process should be contacted during working hours.
3.8 Role of Coroner’s Officers
Coroners Officers have knowledge of the Coronial system and involvement with families when a child has died unexpectedly. They have a valuable contribution to the information sharing process and assist and advise with the management of samples and investigations. Once the post-mortem report is available, the Coroner’s Officer will share the findings with the parents, unless the Police request otherwise.
3.9 Role of Coroner and Pathologist
After death the Coroner has control of the body and mementoes/medical samples must not be taken without their approval.
The post-mortem will be carried out using either a specialist paediatric pathologist or a Home Office forensic pathologist. If the Coroner is concerned about the nature of the death, he may instruct that both a paediatric pathologist and a Home Office pathologist carry out the post-mortem. The Coroner has the choice of pathologist.[5] If during the post-mortem the paediatric pathologist becomes concerned about suspicious circumstances, they must halt the post-mortem and, with the Coroner’s authority, arrange for contact to be made with a Home Office pathologist. The Police must also be notified immediately.
The Coroner’s Officer will ensure that all relevant professionals are advised of the time/date/location of the post-mortem. The SIO will arrange for a Scenes of Crime Officer (SOCO) and an exhibits officer, if relevant, to also attend if the post-mortem is being carried out by/with a Home Office pathologist. The Coroner’s Officer will also advise the parents of the post-mortem details and the right to be represented at the post-mortem.
It is very important that the Pathologist receives a detailed history of the case in advance of the post-mortem examination. As a minimum the ‘History Record’ should be provided to the pathologist. However, the Paediatrician and the SIO are also expected to notify the Pathologist of all and any matters that may be germane to the child’s death. This might mean in some instances that a phone call/email will suffice; in other instances, it might mean that photographs or video recordings are made available to the Pathologist.
At the post-mortem the pathologist will arrange a number of investigations to be carried out. This will include a full skeletal survey for infants and the collection of samples for microbiology and metabolic investigations. This can only be done with the consent of the Coroner and must be only to ascertain the cause of death. The only exception is where the samples are taken by the Police under the Police and Criminal Evidence Act (PACE). If the Paediatrician has commissioned any investigations prior to death the pathologist will need to be advised and the results forwarded to him/her when known.
See appendix A and B for details of specimens to be taken ED.
This protocol supports the Royal College of Pathologists’ ‘Guidelines on Autopsy Practice’ (2002), which state that:[6]
- A provisional report (to include a preliminary cause of death where possible) should be sent out within 5 working days of the examination.
- Where there are no complex investigations the complete report should be sent out within one week of the examination.
- Results of further investigations with a commentary or conclusions and the stated cause of death should be sent out within one week of availability of those findings.
The provisional report to the Coroner will also include details of retained samples. Under Rule 10(1) Coroners Rules 1984, the person undertaking the post-mortem must report to the Coroner. This means that the report will always be forwarded to the Coroner in the first instance, and only at his/her discretion will it be shared with partners. In practice, local Coroners will allow the post-mortem report to be shared with the Police, CDOP Manager and Designated Doctor for Child Deaths once he/she has had an opportunity to review the findings and decide on any further course of action.
3.10 Role of Local Authority
3.10.1 Social Care
It is important that Social Care are consulted at the beginning of this process to ascertain any prior knowledge of the child, siblings and family. If the family are known to social care or there are concerns regarding the needs or safety of other children social care will be involved in the multi-agency case management discussion. The Emergency Duty Team should be notified of the unexpected death out of hours (01733 234724) and the normal referral process for social care should followed during daytime hours.
The level of involvement will differ markedly dependant on the circumstances, the case history and any safeguarding issues raised in respect of the siblings. If there are concerns about deliberate harm, Social Care must be contacted immediately in order to ensure the safety of remaining siblings.
3.10.2 Education
Education services will be involved in the case management discussions if the child or siblings are of school age.
Other children and adult services may also be required to have input into the multi-agency response (e.g. mental health or substance misuse workers, early years, children centres, the Youth Offending Service etc).
4. Multi agency response
4.1 General
So far, the protocol has detailed the actions of professionals who attend when a child is found dying or dead and the actions to be followed when the child is received at the Emergency Department.
Once the death has been confirmed, any specimens or samples taken and the history has been taken, the following also need to be done.
4.2 Informing the Co-ordinator for Child Death Overview Panel (CDOP) Arrangements
The Safeguarding Childrens Partnership must be informed about the child death via the CDOP Manager. A Form A Notification must be sent via the eCDOP public site: https://www.ecdop.co.uk/CambridgeshirePeterborough/Live/Public
From this point the Child Death Review Form B should be used to collect relevant details. See Safeguarding Childrens Partnership ‘Protocol and Terms of Reference for the Child Death Overview Panel for Cambridgeshire and Peterborough Safeguarding Childrens Partnership’.[7]
- The decision to undertake a home visit should be agreed between the Protecting Vulnerable People directorate or Duty Detective Inspector and the on-call Rapid Response paediatrician during on-call hours. A visit would normally occur in SUDI cases or where it was agreed that it would likely yield valuable information regarding cause of death, or with safeguarding considerations.
- The initial scene of death visit is most commonly at the home of the child but may not be. However, the visit is an essential part of the multi-agency investigation into an unexpected child death to establish the circumstances of death especially if a child has died in a non-hospital setting.
- If the scene of death has been designated as a crime scene by the Police a joint visit should not automatically be precluded but should be given careful consideration.
- Prior to the visit the Police Officer and Health professional should exchange any known information about the child and family, and plan how to conduct the visit. It is essential that any records completed surrounding the incident and particularly the recent health records are accessed. This will prevent duplication of questions to the bereaved parents/carers.
- It is possible for the visit to take place in two parts; if the family are not present at the scene of death and / or do not wish to return there the interview can take place in their current location and the scene of death assessed separately.
- The visit should almost always take place if a child is under 12 months.
- This is joint health/police (SIO trained) visit and should take place as soon as possible after death is confirmed.
- Information from this visit or the reasoning for not completing a scene of death visit must be shared with the pathologist (when a post-mortem is to be undertaken), the health coordinating team and the CDOP Co-ordinator. Please see appendix F for further guidance on when a home visit is indicated.
- If there has been a section 47 strategy meeting, discussion must take place within Children’s Social Care about whether a scene of death visit is appropriate.
4.4 Plan of Scene of death visit
The purpose of this visit and the discussion with the parents include the following and rely on the skills and knowledge of both the police and health professionals:
- To complete and clarify the history of events.
- Use of health knowledge and understanding of child development and childhood illnesses and their likely causes.
- Identify and contextualise factors that may have contributed to death.
- To provide information and support to the family.
- To identify evidence that implies suspicious circumstances.
- To identify inconsistencies in history.
- To record observations on sleep environment.
- To consider video recording the environment for the benefit of the pathologist – not for evidential purposes.
- To ensure appropriate handling of evidence.
- To ensure legal provisions (principally PACE 1984) are observed.
- Room measurements would usually be the prerogative of the Police / SOCO. Exact measurements of room temperature will not normally need to be taken but a comment if the room is excessively hot or cold can be added to the observations.
Both Police and Paediatrician are required to use the Safeguarding Childrens Partnership Form B to record findings to date.
4.5 Initial Case Management Discussion
Information sharing is vital; therefore, the appropriate health professional, Police and Social Care participate in an Initial Case Management Discussion, within 12 hours of the death being confirmed. This may be a meeting or telephone conference. Agreed actions and who is responsible for them must be recorded and forwarded to the CDOP Manager. Information should be shared on the following:
- background information/presentation of child
- background information regarding child/siblings/carers
- safeguarding issues of surviving siblings
- immediate Child Protection issues
- nature of any suspicions
- consider request of blood samples from parents/carers
- scene management
- contact with Coroner
- timing of PM and briefing of pathologist
- restrictions on viewing of body
- significant Police action (arrests, statements)
- immediate support for bereaved – deployment of Family Liaison Officer
- coordination of Professionals Contact with family – home visit
- agreed point of contact with mortuary and Bereavement staff
- status of enquiry/investigation – criminal / child in need or child in need of protection.
- time and date of SUDI case meeting
- press strategy
- staff Welfare
- notification to CDOP Manager
Where there is a criminal investigation initiated the sharing and disclosure of information remains a key element in the process of the investigation into the child’s death and the meeting should still be held face to face with detailed minutes being taken. Each party at that meeting will be advised that there is a potential that any information shared could be used at a later date in a criminal court. The Police may withhold information from the meeting in order to protect the integrity of any evidence gathered as long as in doing so it does not pose a threat to the health and wellbeing of anyone or is detrimental to the decision making process relating to the safeguarding of siblings or other children.
If a referral has not already been made, and it is the view of this meeting that abuse or neglect is a factor in the death a referral must be made to social services for a Section 47 Child Protection Enquiry, and then to the Safeguarding Childrens Partnership for consideration by the Serious Case Review Panel.
This meeting must be minuted.
4.6 Second Case Management Discussion
The second case discussion is to be convened shortly after the initial post-mortem results become available. This may be by telephone and possibly not be needed for all unexpected deaths but should occur when the preliminary results of the post-mortem are available. The meeting will be organised by the CDOP Manager. All known professionals who have knowledge of the family will be invited and it will be convened in a venue suitable for the majority of the professionals.
The aim of this meeting is to consider any child protection or other needs of surviving children and any other children; ensure the bereavement needs of the family are addressed and any contributing factors to the death identified.
To facilitate this, the meeting will review the information and the actions of the initial discussion and gather detailed information from other professionals. The meeting will be minuted and any key actions identified to form a plan which will be reviewed at the final case discussion. A copy of the minutes taken will be distributed to all professionals involved, including the Coroner. A provisional date for the third case discussion meeting is made for 12 weeks’ time.
Agenda
Information Sharing and Bereavement Planning Meeting
(Agenda for Chair and minute taker)
1. | Introductions and Apologies |
2. | Purpose of meeting To share information, co-ordinate a bereavement plan for the family and identify whether there are any safeguarding concerns. Explanation of rapid response process. |
3. | Information Sharing |
4. | Safeguarding Risks / Issues? This needs to be minuted even if there are none. |
5. | Bereavement plan A named lead person to support the family should be identified rather than a professional’s title. |
6. | Communication with the family § The Coroner’s officer is responsible for informing parents of the post-mortem results. Consider if parents would like support from a known (health) professional for this. § Have parents been given leaflets, have they been informed of this meeting / further process and CDOP |
7. | Notification of Other Agencies Ensure all relevant agencies / professionals have been notified of the child’s death |
8. | Serious Case Review consideration Do those present feel criteria are met for a SCR? |
9. | Final report to Child Death Review Committee Explain further process: final case discussion, completion of form C, CDOP panel |
10. | Future Meetings (usually held approx. 6-8 weeks after initial meeting) Set a date for the final case discussion, date to be confirmed when post-mortem results received. |
4.7 Third Case Management Discussion
This may be held when the final post-mortem results are known.[8] This will normally be a meeting not a telephone discussion, however some flexibility is allowed given the differences between cases. Where the post-mortem provides a conclusive cause of death with no contributory factors and little potential for learning, no meeting is necessary. Otherwise parties will meet for the third case management discussion which is arranged and chaired by the designated professional or by a member of the Rapid Response team.
There needs to be an explicit discussion about the possibility of abuse or neglect either causing or contributing to death. If no evidence of maltreatment is identified the minutes shall record this.
The minutes of this meeting will be in the completion of the Form C, Analysis Proforma with the approval of all attendees then sent to the Coroner.
If it is the view of this meeting that abuse, or neglect is a factor in the death a referral must be made to the relevant Safeguarding Childrens Partnership Serious Case Review Panel.
5. Governance
5.1 Safeguarding Childrens Partnership Audit Responsibilities
The Cambridgeshire Safeguarding Childrens Partnership and Peterborough Safeguarding Childrens Partnership will:
- Observe the statutory obligations within Chapter 5 of Working Together to Safeguard Children 2015
- Monitor and review audits, to comply with DFE data collection and to demonstrate the protocol is being followed.
- Receive a report on a regular basis from CDOP
5.2 Accountability
Partner organisations will be accountable to the Safeguarding Childrens Partnerships for their organisation meeting its responsibilities under this protocol through representation on CDOP.
Accountability will be with named posts not an individual. To carry out its statutory child death review function, the Safeguarding Childrens Partnerships need to be informed of any changes to the identified posts. Therefore, the following agencies are required to inform the Safeguarding Childrens Partnership Coordinator for child death arrangements of the relevant details for their representation:
- Cambridgeshire Constabulary
- Cambridgeshire and Peterborough Clinical Commissioning Group
- East of England Ambulance Service NHS Trust
- Cambridge University Hospital NHS Foundation Trust
- Hinchingbrooke NHS Health Care Trust
- Peterborough and Stamford Hospitals NHS Foundation Trust
- Peterborough Children’s Services (Social Care)
- Cambridgeshire County Council – Children and Young People Services (Social Care)
- Coroner for Peterborough
- Coroner for North and East Cambridgeshire
- Coroner for South and West Cambridgeshire
The relevant CDOP member will assume responsibility for ensuring their agency is aware of:
- Awareness raising and publicity.
- Identifying and addressing internal agency training needs and advising the Safeguarding Childrens Partnership with regards to need for interagency training.
- Ensuring this protocol is observed within their organisation.
- Advising the Safeguarding Childrens Partnerships of suggested amendments to the protocol.
- Highlighting and reconciling conflicts within their organisation arising from this protocol.
- Addressing the availability and accessibility of staff.
Appendix A – Protocol for Deceased Children Presenting to the Emergency Department – Cambridgeshire
Guideline
Deceased children presenting to the Emergency Department
1 Scope
Emergency Department (ED)
2 Purpose
To clarify management of deceased children in the Emergency Department in line with national and regional recommendations.
3 Introduction
Deceased children in the Emergency department fall into two categories: children admitted as an emergency where active resuscitation is still ongoing and children where attempts at active resuscitation are clearly inappropriate or have stopped prior to arrival in ED.
Children who are actively resuscitated require investigations and assessment in line with national recommendations and the process is outlined below. This will almost exclusively occur in the paediatric resuscitation area of the ED.
Children who are found dead outside hospital (excluding road traffic collisions or obvious accidental trauma) and where resuscitation either is clearly inappropriate or has stopped prior to arrival will also require assessment and investigations by a paediatrician before transfer to the mortuary. As a matter of principle this will be performed by a senior paediatrician in the ED. At times of high activity this can be challenging, and an alternative location may have to be found. During office hours this could be in the mortuary and – if the child is accompanied by parents (they may choose not to accompany their child) – possibly in the chapel of rest. However, this will need prior discussion with mortuary staff/technicians.
Under no circumstances should these children be assessed (and specimens taken) anywhere outside the Emergency Department or mortuary due to the constraints posed by the Human Tissue Act licence.
Investigations
Sample | Handling | Test | Purpose |
Blood Cultures | Microbiology If insufficient blood, aerobic only | Culture & Sensitivity | Identification of infection – desirable to collect as soon as possible as delays may make interpretation difficult. It is acceptable to obtain this with a ‘cardiac stab’. |
CSF | Microbiology – CSF samples should not be taken if any suspicion of cranial trauma | Microscopy, Culture& Sensitivity | Identification of infection – desirable to collect as soon as possible as delays may make interpretation difficult. One attempt at a lumbar puncture to be attempted and document if this is not successful |
Nasopharyngeal aspirate | Virology | Viral cultures, immunofluorescence and DNA amplification techniques | Identification of viral infections |
Nasopharyngeal aspirate or throat swab | Microbiology | Culture & Sensitivity | Identification of infection |
Appendix B – Protocol for Deceased Children Presenting to the Emergency Department – as agreed by HM Coroner
Detailed history and Examination
History
- Presenting History: record parents’ accounts of events. Ideally, information should be recorded verbatim- use their own words as far as possible. Detailed history as for any critically ill child.
- Basic details of baby/child, the parents, and other family members.
- A narrative account of the 24 hours leading up to the child’s death. Unexpected death In children less than 2 yrs. age, a full description of when and how the baby slept and fed, any activity, who was with the baby at different times, the baby’s health and activity levels, the final sleep and any changes to routine. Where and how the baby was sleeping, clothing, bed coverings, position; any changes in that during the course of the night; if bed sharing, who else was in the bed and their positions relative to the baby; when and by whom the baby was checked during the sleep; description of the last feed and any night time feeds; heating and ventilation.
- Where and how the baby was found, position, coverings, appearance and any unusual features; any action taken after the baby was found.
- Past medical history, including pregnancy and delivery, birth weight, post-natal problems, growth and development, normal routine and feeding, any illnesses, immunisations , medications, drug allergies, routine surveillance; Also details of normal routine for the baby, including feeding, sleeping patterns and practices. Check previous OPD/ hospital, A and E, HV and GP visits
- Family medical history, including any medical or psychiatric history of the parents and other immediate family members; infectious contacts; any history of respiratory, cardiac, neurological disorders or metabolic disorder in the family and any previous infant or other sudden deaths in the family. The second twin MUST be examined and investigated appropriately by the Paediatrician
- Social history, family structure and dynamics, housing, use of alcohol, recreational drugs, and tobacco; parents’ occupations; any social services involvement in the past, including any child protection concerns.
Examination
- A detailed examination depends of the clinical presentation
- In unexpected deaths: Consider the following
- Head to toe examination and front to back for bruising/injuries/ visible signs of bleeding/discharge: use body diagrams to document the injuries (Sheet C of the UHL Standard Child Protection Paperwork)
- Examination: spine, skull, chest, upper limbs, lower limbs, genitalia, anal region
- Abdomen: Hepatomegaly
- Signs of dehydration, Rectal temp, Wt./Length/HC, State of nutrition and cleanliness
- Petechiae in distribution of SVC
- Eye exam: retinal haemorrhages
- Pre-intubation mouth exam. ENT exam: frenulum/ bleeding/pink fluid from the nose. Frothy fluid, commonly bloodstained, is often present around the nose and or mouth and its presence should be documented.
- Sites of medical intervention: Example: IV lines, IO lines etc needs to be documented
- The presence of any discolouration of the skin, particularly dependent livid. Skin livido and pallor from local pressure (e.g. on the nose in a child who has been face down).
Samples
Initial samples to be taken immediately after sudden unexpected death in infancy/Children (SUDIC)
- No samples in NAI cases or suspected NAI cases.
- Consent: for post-mortem tissue samples, a fully informed consent must be obtained from the parent or carer with parental responsibility and this must be clearly documented
- Blood samples taken DURING AND AFTER Resuscitation: Maintain strict chain of evidence for all the samples taken (chain of evidence forms-Appendix 7). No samples should be sent via the CHUTE.
- Please Fax a copy of this to the coroner, pathologist and the SUDIC paediatrician.
- No supra-pubic punctures should be attempted for urine samples.
- Urine/stool stained nappy should be preserved and sent for analysis
“Practice Note – Examination of the body following the unexpected death of a child” (11 April 2011) Dr Richard Brown – (at that time; Named Doctor for Safeguarding Children, Peterborough).
As soon as is practicable following the cessation of resuscitation, the baby or child should be examined by the consultant paediatrician on call (in some cases this might be together with a consultant in emergency medicine or, for some young people over 16 years of age, the consultant in emergency medicine may be more appropriate than the paediatrician). A detailed and careful history of events leading up to and following the discovery of the child’s collapse should be taken from the parents/carers. The purpose of obtaining high quality information at this stage is to understand the cause of death when appropriate and to identify anything suspicious about it. The paediatrician should carefully document the history and examination findings in the hospital notes. This should include a full account of any resuscitation and any interventions or investigations carried out. A narrative account by the carer of the events leading to death should be documented.
The examination findings, including any post-mortem changes, should be documented on a body chart. Any opinion communicated to police or children’s social care regarding such post-mortem changes should be framed within the context of the paediatrician’s experience and training.
Appendix C – Organisations Contact List
Designated Doctor for Deaths in Childhood
Cambridgeshire and Peterborough
Cambridgeshire Community Services
Block 13 Ida Darwin
Fulbourn
CB21 5EE
Tel: 07534980967
Child Death Review Manager
Cambridgeshire and Peterborough
Jenny Valentine
Cambridgeshire and Peterborough Clinical Commissioning Group
Lockton House
Clarendon Road
Cambridge CB2 8FH
Generic CDOP inbox: CAPCCG.cdop@nhs.net (secure)
Cambridgeshire and Peterborough Safeguarding Partnership Board
http://www.safeguardingcambspeterborough.org.uk
Tel: 01733 863744
Cambridgeshire Social Care Contact Centre
0345 045 0180
Peterborough Social Care Contact Centre
01733 864180
Cambridgeshire / Peterborough Social Care Emergency Duty Team
01733 234724
Cambridgeshire Constabulary
Police Headquarters
Hinchingbrooke Park
Huntingdon
PE29 6NP
Tel: 101 or 01480 456111
BEREAVEMENT ORGANISATIONS
East Anglia’s Children’s Hospices (EACH)
Bereavement support for children and families in Cambridgeshire and Peterborough
Church Lane
Milton
Cambridge
CB24 6AB
Tel: 01223 815115
Email: reception@each.org.uk
Web: www.each.co.uk
STARS Children’s Bereavement Support Services (Cambridgeshire)
42 High Street
Milton
Cambridge
CB24 6DF
Tel: 01223 863511 Mobile: 07827 743497
Email: info@talktostars.org.uk
Web: www.talktostars.org.uk
The Child Bereavement Trust
Aston House, High Street
West Wycombe
High Wycombe
HP14 3AG
Tel: 01494 446648
Email: enquiries@childbereavement.org.uk
Website: www.childbereavement.org.uk
Child Death Helpline
Child Death Helpline Administration Centre
York House
37 – 39 Queen Square
London
WC1N 3BH
020 7813 8416
0800 282986
The Lullaby Trust (previously The Foundation for the Study of Infant Deaths)
Bereavement support
Helpline: 0808 802 6868
Monday – Friday 10am-5pm
Weekends and public holidays 6pm–10pm
Tel: 01480 812778
References
[1] Child Death Review- Statutory and Operational Guidance (England) October 2018
[2] Office for National Statistics. Vital Statistics: Population and Health Reference Tables. 2017. https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/vitalstatisticspopulationandhealthreferencetables
[3] Working Together 2015 Para 5.12
[4] Sn 8(1) Coroners Act 1988
[a] A Guide to Investigating Child Deaths ACPO 2014
[5] Rule 6(1) a Coroners Rules 1984
[6] Royal College of Pathologists Guidelines on Autopsy Practice (2002)
[7] www.cambslscb.org.uk and www.pscb.org.uk
[8] Working Together 2015 Para 5.25
