Table of Contents
Referral of Child and Young Persons to the Sexual Assault Referral Centre (SARC)
Key points for professionals
- A disclosure is not required for a Child Sexual Abuse Medical around suspected Sexual Abuse or Exploitation to take place.
- The process begins at the point of a referral to the Police (MASH) and/or Children’s Social Care who will identify cases and Mountain Healthcare should be invited to all Sexual Abuse or Exploitation strategy meetings to assist the multi-agency decision-making.
- Non acute Child Sexual Abuse Medicals are conducted in a child and young person friendly way and professionals should avoid making assumptions on procedures in their decision-making.
- Child Sexual Abuse Medicals are more than a physical examination, they assess the emotional needs of the child and ensure wrap around services support the child or young person beyond what may be available to Police and Social Care.
The Child Sexual Abuse Service is available at the SARC: this provides holistic assessment for children and young people who have experienced some form of sexual violence.
- Allows assessment of the needs of children and access to the wrap around services of the SARC.
- Enables documentation of injuries and the undertaking of forensic evidence to support the criminal justice system.
- Considers screening for sexually transmitted infection.
- Provides reassurance for findings ensuring the child, young person and their family are informed that they are normal and that there will be no long-term consequences for their experience.
- Provides a central hub of expertise and collates performance data for commissioners to identify best practice and gaps in service provision.
- Provides Sexually Transmitted Infection (STI) screening for all under 13’s as part of the holistic assessment (those over 13yrs are referred to iCASH)
- The SARC do not carry out Female Genital Mutilation examinations. Please follow your local commissioned pathways
Access to the SARC should not be driven by disclosure only as it well established that many children do not disclose, have normalised their experience or do not recognise abuse, therefore lack of disclosure should not be a barrier to accessing services.
1. Introduction
The purpose of this policy document is to outline the process for referring Children and Young Persons (aged up to 18 years) to the Peterborough and Cambridgeshire Sexual Assault Referral Centre (SARC).
To assist professionals understanding, the term SARC medical will be replaced with the term Child Sexual Abuse Medical for children and young people who have experienced sexual abuse or exploitation.
A Child Sexual Abuse Medical should always be considered according to the guidelines set out in The Royal College of Paediatrics and Child Health, specifically the Faculty of Forensic and Legal Medicine (FFLM). The guidelines states there are 3 occasions when a Child Protection Medical will be required
- a child has made an allegation of sexual abuse or
- sexual abuse has been witnessed or
- when a referring agency strongly suspects abuse has occurred.
The Child Sexual Abuse Medical should be seen to at the point of a referral to the Police (MASH) and/or Children’s Social Care who will identify cases and Mountain Healthcare should be invited to all Sexual Abuse or Exploitation strategy meetings to assist the multi-agency decision-making. This will ensure opportunities to follow FFLM guidelines and consult with Mountain Healthcare Paediatric Forensic Medical Examiner/ Forensic Nurse Examiner are maximised. However, the SARC are happy to offer advice to clinicians to aid in a referral being made and support decision making.
This policy document is not to replace any terms of reference or standard operating procedure regarding the running of the SARC or processes once a child or young person has been referred to the SARC.
Any process to refer a child or young person to the SARC must have the child or young person’s welfare at the centre. Although each agency involved with a child or young person has its own protocol, any such decision to refer them to the SARC is a joint agency decision and a strategy meeting is necessary.
When a Child Sexual Abuse Medical has been agreed to be in the best interest of the child or young person, for non-acute cases these should be booked into the established clinics by the authorised referring agencies, and a social worker and/or police officer identified to attend with the child.
Where a child under 13 years, in an acute case, needs to be seen outside of ordinary clinic times for forensic sampling or injury documentation, there is a requirement to seek approval. The need for this examination in these circumstances requires the prior authority of the duty Protecting Vulnerable People Department (PVPD) Detective Inspector, or in their absence, the duty Detective Inspector.
The decision to refer a child or young person to the SARC is a multi-agency decision made during a strategy meeting and in conjunction with a Paediatric Forensic Medical Examiner / Forensic Nurse Examiner from Mountain Healthcare. In the event of a disagreement over a decision, then the safeguarding board policy of “resolving professional differences” will be followed.
Although not limited to; the processes for referring a child or young person to the SARC must consider the protocols of working together (2018), commissioning framework for adult and paediatric sexual assault referral centres (SARC) services, service specification for the clinical evaluation for children and young people who may have been sexually abused (2015) and the NHS National Strategic Direction for Sexual Assault & Abuse Services – Lifelong care for victims and survivors: 2018 – 2023.
A strategy meeting or a multiagency discussion (conference call) is vital. Child Sexual Abuse is a complex assessment. Circumstances such as parental conflict, failure to provide protective parenting, looked after children, as well as understanding of medical history and wider needs of children and their family are vital prior to assessment. No examination should be undertaken without this understanding.
In addition, strategy meetings also allow consideration of:
- Timing of Child Sexual Abuse Medical (FFLM Sexual Offences Prepubertal complainants and Post pubertal Complainants)
- Venue – consideration whether hospital Paediatric Department is required or if other venues are appropriate.
- Consent – Parental Responsibility and Gillick Competence *
- Support – are there any communication barriers which need addressing and who should be present – for young people this could be a person they trust, for ASD, a key care worker or an interpreter for those with English as a second language.
- Police are required for forensic Child Sexual Abuse Medicals, whereas social care must be present for non-acute cases. There is a statutory obligation to safeguard and promote the welfare of vulnerable children and adults and it is felt that a Child Sexual Abuse Medical requires their support even where there no immediate safeguarding issues.
*Parental Responsibility – even where Local Authority share parental responsibility, it is considered best practice to seek consent from the person who holds PR. Only where all attempts have been considered futile, will there be consideration of an examination.
When a decision has been made to refer a child or young person to the SARC, it is necessary to consider the appropriate arrangements for any subsequent clinical examination and support services. Clear referral pathways are established with the SARC service provider, and there is a need for discussion with them at any point a referral is being considered to ensure consultation with the appropriate specialist paediatric medical practitioner or wider services has been facilitated.
Although this guidance refers to all cases of abuse and sexual exploitation relating to a child or young person, where the allegation is that of rape (or attempted rape) from the outset and is an acute case, these are to be referred directly to the SARC via the healthcare service provider (Mountain Healthcare) so the Child Sexual Abuse Medical procedures can be commenced. It is important that a strategy meeting/multiagency discussion is undertaken, however where time restrictions are felt to impact on forensic evidence or delays are caused which results in additional distress to the child or young person, the examination will take place prior to the meeting. Mountain Healthcare have an obligation in these circumstances to complete an Incident Report which is shared with commissioners and discussed at the SARC Operational Group for review and any identified partnership learning. These cases will still to be subject to a full strategy meeting, but it will not delay the medical arrangements and should run parallel to the medical examination taking place.
If a child is deemed to have injuries it is vital that these injuries are assessed and treated in a hospital environment before the child is brought to the SARC. In rare circumstances the forensic medical examiner may need to attend hospital.
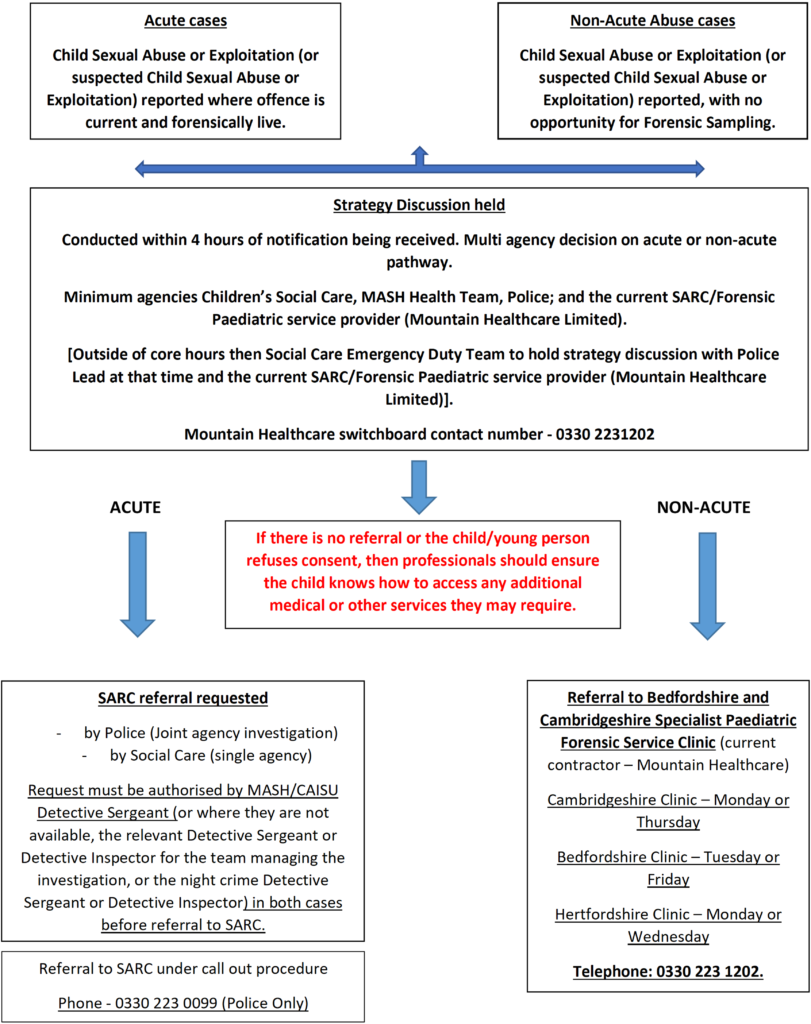
2. Acute Cases
A Forensic acute case is where Child Sexual Abuse or exploitation (or suspected Child Sexual Abuse or exploitation) is reported as follows:
- offence suspected as being vaginal and having taken place in a post pubescent child within 7 days and a pre-pubescent child within 3 days; or
- suspected as being digital or oral within 48 hours; or
- suspected as being an anal assault within 3 days.
If the child has not washed since the time of assault forensic samples should be considered for up to 7 days for digital and anal assaults. If injuries are present this would also be considered an acute case, even outside these timeframes. These time constraints are key and offer the most likelihood of any forensic recovery and documentation of injuries that would stipulate the consideration of an immediate forensic medical examination.
To ensure the most appropriate approach to these cases, with the child or young person’s best interests being the primary consideration, a strategy discussion is to be conducted within 4 hours of any such notification.
Strategy meetings will take place as follows:
- Monday to Friday 0900-1700hrs; Normal strategy meeting procedures to be followed including a representative from Mountain Healthcare
- Out of above hours, weekends and bank holidays; Professionals from EDT, Police and Mountain Healthcare.
N.B. Consideration should be given to inviting the referrer directly even if their agency is already represented i.e. GP, Emergency Department doctor, teacher etc
Where following the strategy discussion it is identified that a Child Sexual Abuse Medical is necessary, and this examination is to take place within the SARC, this is to be directed to a MASH or CAISU Detective Sergeant (or where they are not available, the relevant Detective Sergeant or Detective Inspector for the team managing the investigation, or the night crime Detective Sergeant or Detective Inspector) for discussion on progression. Consultation will be held with the current SARC service provider (Mountain Healthcare Limited either during the strategy meeting or via their call out number 0330 223 0099) to establish the options available for the examination to take place within current prearranged clinic times, or where necessary the need to call out additional SARC specialist resources. This will be considered in line with the child or young person’s best interests and the evidential necessity to take alternative action outside of prearranged clinic times.
If the decision is for no referral to be made to the SARC, or the child/young person refuses to consent to any examination, then the lead professionals must ensure communication to the child/young person, to ensure they know how to access any additional medical service (including contraception and sexual health if appropriate) or other support service they may require. If over 13, a child may choose to self-refer later after initial refusal therefore information on how to contact SARC should be provided.
During any Child Sexual Abuse Medical at the SARC, if injuries are noted outside the capture of this specialist examination, then the CAISU DS should be consulted for a decision on whether further evidence capture is required i.e., SOCO attendance at the SARC to photograph. Every effort should be made to avoid multiple examinations of the child or young person.
The provision for acute Child Sexual Abuse Medical examinations is available Monday to Friday. This is a tri-force service (Bedfordshire, Hertfordshire and Cambridgeshire) and whilst every effort will be made for the medical to take place at the child or young person’s closest SARC, there may be occasions where travel is required. This may have to be facilitated by Police or Social Care.
Regionally, there is provision for acute Child Sexual Abuse Medicals to be undertaken on a Saturday morning via NHSE services and the procedures documented in this pathway should be followed as normal. Mountain Healthcare remain the dedicated point of contact for referrals.
3. Non-Acute Abuse Cases.
Where Child Sexual Abuse (or suspected Child Sexual Abuse) is reported, with the offence not having occurred within the timeframes to identify it as an acute case, this is said to be a non-acute case (previously known as chronic or holistic). These cases have no opportunities for forensic recovery, however there is still a need for consideration of medical examination, for the health and well-being of the child or young person as well as identifying potential evidence of the alleged abuse.
Children and young people are likely to have beliefs about their situation, even where they have not disclosed and it is important that they have the opportunity to be told about their bodies, have screening for sexually acquired infections and to be able to access wrap around services, to reduce long term sequelae for child sexual abuse.
To ensure an appropriate approach, a strategy discussion is to be conducted within 4 hours of any such notification.
Strategy meetings will take place as follows:
- Monday to Friday 0900-1700hrs; Normal strategy meeting procedures to be followed including a representative from Mountain Healthcare
- Out of above hours, weekends and bank holidays; Professionals from EDT, Police and Mountain Healthcare.
N.B. Consideration should be given to inviting the referrer directly even if their agency is already represented i.e. GP, Emergency Department doctor, teacher etc
Where it is decided following the strategy discussion a Child Sexual Abuse examination is necessary, then contact is to be made with the service provider (Mountain Healthcare Limited) for the child or young person to be referred to one of their Specialist Paediatric Forensic Service Clinics. These are currently held at the Cambridgeshire SARC on Mondays and Thursdays , the Bedfordshire SARC on Tuesdays and Fridays and the Hertfordshire SARC on Mondays and Wednesdays.
Should there be any professional difference on whether to open the SARC for a Child Sexual Abuse Medical, the circumstances of the case, the outcome and the rational for that decision are to be passed to the Protecting Vulnerable People Department (PVPD) Detective Chief Inspector, for an appropriate review to be completed and a serious incident form completed and sent to NHS England by Mountain Healthcare.
If the decision is for no referral to be made, or the child/young person refuses to consent to any examination, then the lead professionals must ensure communication to the child/young person, to ensure they know how to access any additional medical service or other support service they may require.
In the event of a disagreement over a decision, then the safeguarding board policy of “resolving professional differences” will be followed.
4. Ongoing Information Sharing and Referral
On attendance at the SARC, a Child Sexual Abuse Medical will be undertaken and include wider safeguarding needs, risks of sexually acquired infections, assessment of emotional and mental health needs and consideration of needs of parents, siblings and peers.
Consent is undertaken by the examiner from the person with parental responsibility or the Gillick Competent young person and no information will be shared without their full understanding of what information is shared and who this will be shared with.
Following the Child Sexual Abuse Medical, case reports are completed and shared with Police and Social Care. In the event an evidential MG11 is required, the SARC/Police protocol will be followed.
All children and young people will receive a follow-up safeguarding referral if the social worker is not present – even in under 13s, the safeguarding referral should have a summary of the examination findings which are relevant in order these are on file.
All children and young people will receive a safeguarding alert sent to the named Safeguarding Nurse – this will then be shared with Looked After Children’s Team, CAMHS, health visiting, school nurse as appropriate.
All children and young people will have a notification letter sent to GP.
All children and young people will have a sexual health care plan to include a referral for screening. This will be to ICASH for 13s and overs. For children under 13 STI screening will be provided at the SARC (currently Cambridgeshire and Hertfordshire)
5. Follow Up
The SARC examiner will share at the time the finding with the Social Worker and document in the medical records. Safeguarding concerns are completed via a follow-up referral (as per 4.3). For those under 13yrs, a report is shared within 3 weeks to allow a comprehensive review of the examination and any additional screening which had been completed. This is the contractual timeframe but for cases which require an urgent report, a request can be made and will be completed as soon as possible. For those aged 13-17yrs, a report will be provided following the agreed request process.
Safeguarding professionals must consider whether further Child Sexual Abuse Medicals are required for siblings or the wider familial network. This should not be reliant on disclosures, but of a contextual assessment of the circumstances including the Child Sexual Abuse Medical outcome. Consideration of further strategy discussion should be made to ensure this is a multi-agency decision.
6. Accountability
It is expected that all agencies embed and adhere to the principles and processes outlined in this document.
Accountability will be assessed through multi-agency audits and feedback shared through relevant workstream meetings, operational groups and governance mechanisms.
7. Escalation
In the event of any professional disagreement around thresholds, strategy meeting outcomes or SARC attendance, the Safeguarding Board “resolving professional differences” policy will be followed.
This policy is already well established within Cambridgeshire and Peterborough and ensures consistency in process aligned to other safeguarding decisions.
8. Conclusion
It is of paramount importance that the child or young person is considered at the centre of any decisions that are made with regard to their health and wellbeing. This is no different with any referral considerations to the SARC for examination. This document outlines how this vital support can be accessed, with the child/young person’s best interests in mind and ensure the decision makers involved make referrals to the most appropriate service in conjunction with the current SARC service provider, Mountain Healthcare Limited.
Where there are any concerns or difficulties with any individual case or the service provision, these are to be directed through to Protecting Vulnerable People Department (PVPD) Detective Chief Inspector and a serious incident form completed and sent to NHS England
9. Equality Statement:
All stakeholders and commissioned services involved in supporting clients via the SARC takes personal responsibility to help create an inclusive service. Clients and staff respect one another, feel valued for their differences and can be themselves. We are committed to providing reasonable adjustments, wherever needed so everyone feels welcome and have equal opportunity to access SARC services. We are committed to meeting our legal and moral obligations to promote equality of opportunity, eliminate discrimination, harassment and victimisation and promote good relations.
Referral Process to Specialist Forensic Paediatric Service